Healthcare Payers
Welcome Home.
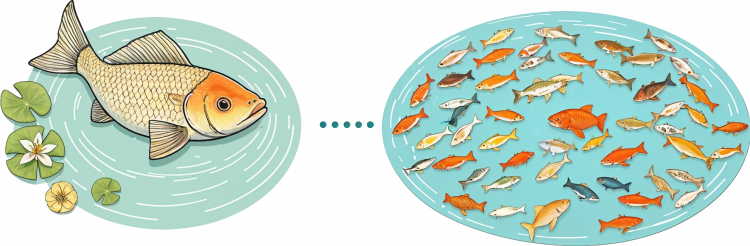
Be the Big Fish in the Little Pond not the Little Fish in the Big Pond
Working with Matridyne you’ll always get our ‘A’ Team. We believe in building long term partnerships and that starts with treating you like our only customer.
What We Do
Operations Optimization
Assessments, Data-Driven Optimizations, ROI Capture

We help healthcare payers streamline workflows, enhance efficiency, and improve compliance. We specialize in optimizing core operational functions such as provider network management, claims processing, enrollment & eligibility, appeals & grievances, and care management.
By leveraging AI, automation, and data-driven insights, we reduce administrative burden, improve accuracy, and enhance STAR ratings and NCQA accreditation performance.
Our solutions address key operational challenges, ensuring seamless coordination between payers, providers, and members while maintaining regulatory compliance. We do this better than anyone by aligning leading Industry Operators with hands-on delivery rockstars to deliver the outcomes and returns you expect.

Backoffice Optimization
Smarter, Faster, More Resilient
We optimize the backbone of healthcare payer operations, ensuring Health Plan Operations run smoothly, predictably, and cost-efficiently. This includes comprehensive support for platform configuration and maintenance, as well as third-party vendor and service provider management, allowing payers to focus on strategic priorities without the friction of operational bottlenecks.
We also recognize that robust IT capabilities are essential for sustaining a high-performing payer ecosystem. Beyond core IT infrastructure—including networks, cloud management, telephony, and end-user technology—we work alongside CIOs to develop and refine IT strategies, strengthen Enterprise Architecture functions, and optimize mission-critical platforms such as Electronic Data Interchange (EDI), Customer Relationship Management (CRM), and Enterprise Document Management (EDM). Our expertise in AI-driven Workflow Automation and Robotic Process Automation (RPA) helps payers eliminate inefficiencies, reduce costs, and improve overall system performance.
For IT organizations, we provide expertise in IT Service Management (ITSM), DevOps, Agile Transformation, and Project Delivery Optimization, ensuring teams are equipped to manage workloads effectively and scale efficiently. We also maintain a strong focus on Cybersecurity regulations and emerging technologies, helping payers stay ahead of evolving threats while maintaining compliance.
As healthcare payer experts, we understand the unique and often competing priorities you face. Our approach balances operational excellence, regulatory alignment, and forward-looking innovation, ensuring payers enhance efficiency, reduce risk, and maximize ROI—all while delivering a better experience for members and providers.
Healthplan Digital Transformation
Future Proofing for Payers & their Members, Providers, & Partners

Data isn’t just a byproduct of operations—it’s the foundation for measuring success, anticipating issues, and ensuring compliance. Without the right data strategy, healthcare payers risk blind spots in performance, financial leakage, and regulatory misalignment. We help payers take control of their data with practical, actionable strategies that deliver real-world impact—not just theoretical insights.
Whether at a strategic level—developing enterprise-wide data frameworks—or at a tactical level, supporting Analytics, Reporting, Automation, and Data Governance, we ensure that payers can extract value from their data, improve decision-making, and stay ahead of regulatory requirements. Unlike firms that operate only in IT or business silos, we bridge the gap between operations, technology, and vendors, ensuring seamless collaboration across all stakeholders.
With deep healthcare payer expertise, we understand payer data better than most—so we can deliver value immediately. Whether working on Risk Adjustment Analytics, STAR Ratings, claims integrity, or Regulatory Reporting, our ability to navigate the nuances of payer data ensures faster results with less friction.

Data Strategy, Analytics, & Insights
Make Data an Advantage – not a Burden
We optimize the backbone of healthcare payer operations, ensuring Health Plan Operations run smoothly, predictably, and cost-efficiently. This includes comprehensive support for platform configuration and maintenance, as well as third-party vendor and service provider management, allowing payers to focus on strategic priorities without the friction of operational bottlenecks.
We also recognize that robust IT capabilities are essential for sustaining a high-performing payer ecosystem. Beyond core IT infrastructure—including networks, cloud management, telephony, and end-user technology—we work alongside CIOs to develop and refine IT strategies, strengthen Enterprise Architecture functions, and optimize mission-critical platforms such as Electronic Data Interchange (EDI), Customer Relationship Management (CRM), and Enterprise Document Management (EDM). Our expertise in AI-driven workflow automation and Robotic Process Automation (RPA) helps payers eliminate inefficiencies, reduce costs, and improve overall system performance.
For IT organizations, we provide expertise in IT Service Management (ITSM), DevOps, Agile transformation, and Project Delivery Optimization, ensuring teams are equipped to manage workloads effectively and scale efficiently. We also maintain a strong focus on Cybersecurity regulations and emerging technologies, helping payers stay ahead of evolving threats while maintaining compliance.
As healthcare payer experts, we understand the unique and often competing priorities you face. Our approach balances operational excellence, regulatory alignment, and forward-looking innovation, ensuring payers enhance efficiency, reduce risk, and maximize ROI—all while delivering a better experience for members and providers.
Healthcare Payer News
-
CMS Rate Increases and the AMA’s Response
January 13, 2025Read More





